
Go to the milConnect website and click on the “Benefits” tab, and then click on “Beneficiary Web Enrollment (BWE)” These enrollment options are for new enrollments, Open Season enrollments, and Qualifying Life Event enrollments.If you have questions or if you have special circumstances, call your regional contractor first to discuss your options.Send enrollment fees (if applicable) with your enrollment form.
Step 2: Complete the Enrollment Application Call first to see if they are accepting new patients.If you don’t have to enroll at a military hospital or clinic, you can select a network provider as your PCM. If you live within 30 minutes, call your regional contractor first.You may have to enroll at a military hospital or clinic if you live within the facility's enrollment area. If you don't list a PCM on your enrollment form, we will select one for you. You may select a military or network provider as your PCM. Step 1: Choose a Primary Care Manager (PCM) Visit the Plan Finder to learn about your other options.Waive your drive time standards and enroll if you live within 100 miles of a primary care manager.If you don’t live in a Prime Service Area, you can: To see if you live in a Prime Service Area, you can: Prime Service Areas were also built around the Base Realignment and Closure sites. They ensure medical readiness of active duty by adding to the capability and capacity of military hospitals and clinics. You don't have to be participating or non-participating all of the time.TRICARE Prime is available in Prime Service Areas Geographic areas in the U.S. Non-network providers can choose to participate on a claim-by-claim basis. Non-participating providers do not agree to accept the TRICARE allowable charge or file beneficiary claims.
#APPLY FOR TRICARE ONLINE FULL#
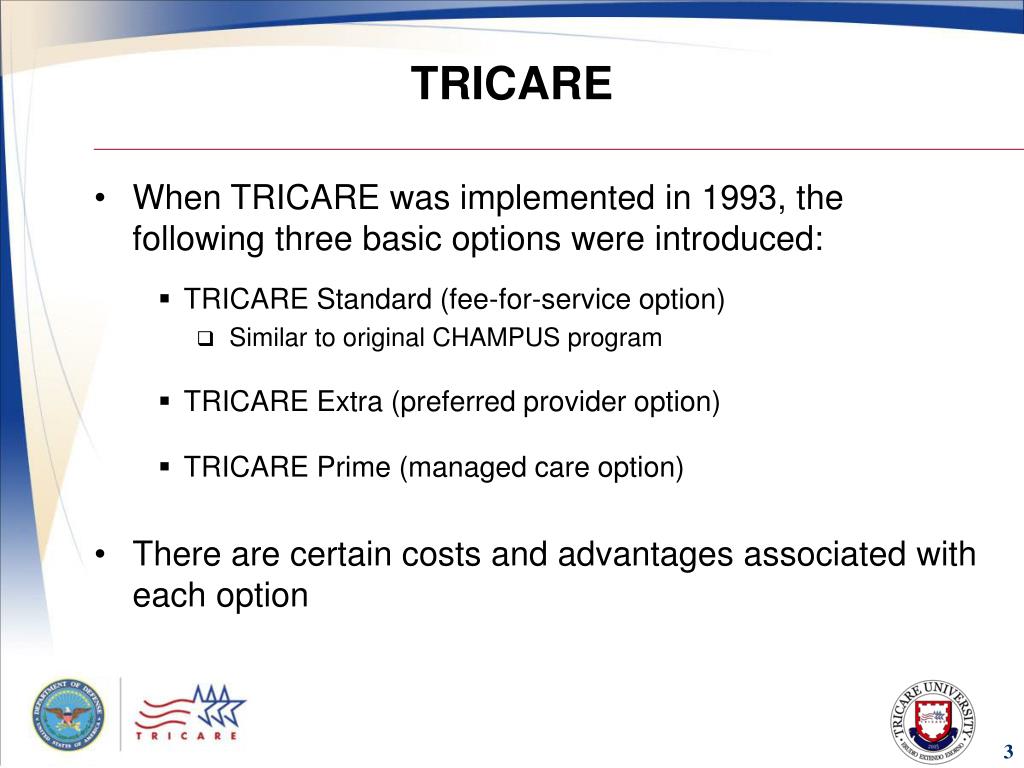
Agree to provide care to TRICARE beneficiaries at a negotiated rate.If you decide to become a network provider, you will sign a contractual agreement with the MCSC in your region. There are two types of TRICARE-authorized providers: Network and Non-Network Providers Network Providers Understanding the different TRICARE provider types will help you decide what type of TRICARE provider you want to be. At a minimum, all TRICARE providers must be authorized/certified under TRICARE Regulation and must have their authorization/certification status verified by the managed care support contractors (MCSCs) in each region. TRICARE defines a provider as a person, business, or institution that provides health care. If you're already a TRICARE-authorized provider or if you want to become a TRICARE-authorized provider, call your MCSC or visit the website, listed below. The MCSCs establish the provider networks and conduct provider education. Managed Care Support ContractorsĮach TRICARE region has its own managed care support contractor (MCSC) who is responsible for administering the TRICARE program in each region. Becoming a TRICARE provider brings with it a higher volume of patients as network providers are placed on the worldwide referral list for all TRICARE beneficiaries. On behalf of the Department of Defense, the men and women of our Armed Forces and their families, as well as our retired families, we want to thank you for your desire to become a TRICARE provider. Being a TRICARE provider means that you're treating America's heroes – the people making sacrifices to keep America strong and safe.


 0 kommentar(er)
0 kommentar(er)
